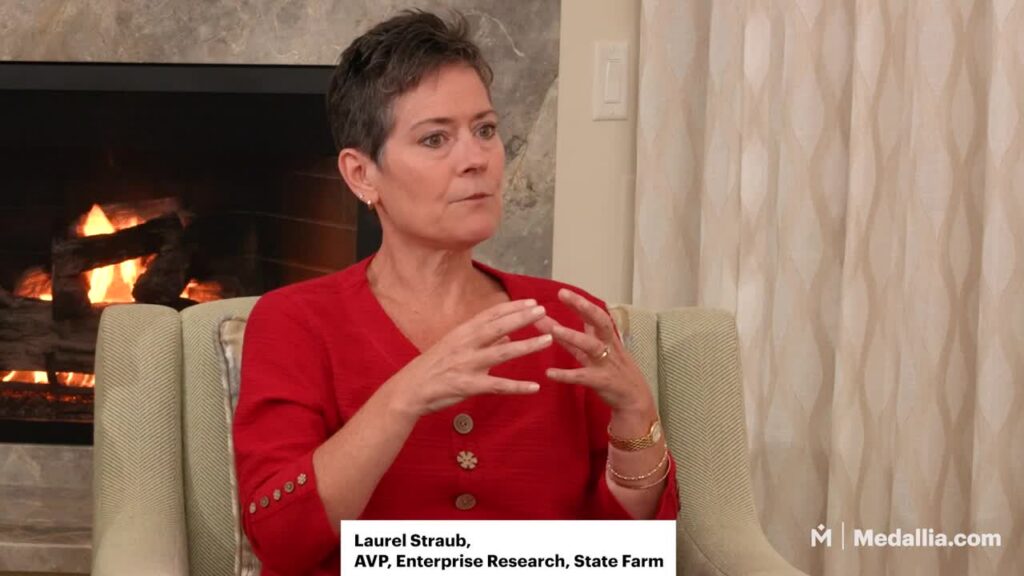
Elizabeth Cleek: [00:00:00] Welcome everyone. I’m Elizabeth Cleek. I’m the Chief Innovation Officer at the Arnold P Gold Foundation and the Arnold P Gold Foundation is an organization whose vision is that healthcare will be dramatically improved by placing the interests, values, and dignity of all people at the core of teaching and practice.
We work to achieve that in three main areas. Education, innovation, and community. We’ve worked with Medallia for the past few years in the innovation space, collaborating to create a six item scale to capture a patient’s experience of their clinical visit. Was it kind, was it safe? Did it feel trustworthy?
And it’s with that lens that I am thrilled to be here with you today and with two fabulous panelists who are emphasizing these values, the values of trust, and putting trust at the core of the work they do in their work. [00:01:00] And so I’m gonna turn it over first to Mike why don’t you tell a little bit about yourself and why you’re here.
Michael Lentz: Great. Thanks Elizabeth. And yeah, just thrilled to be here and good morning everyone. Thanks for attending today’s session. So I am Michael Lentz. I’m the Vice President of Customer Service Operations at Independence Blue Cross, primarily based out of Philadelphia, but we have you satellite offices in the region, also elsewhere in the middle of the country.
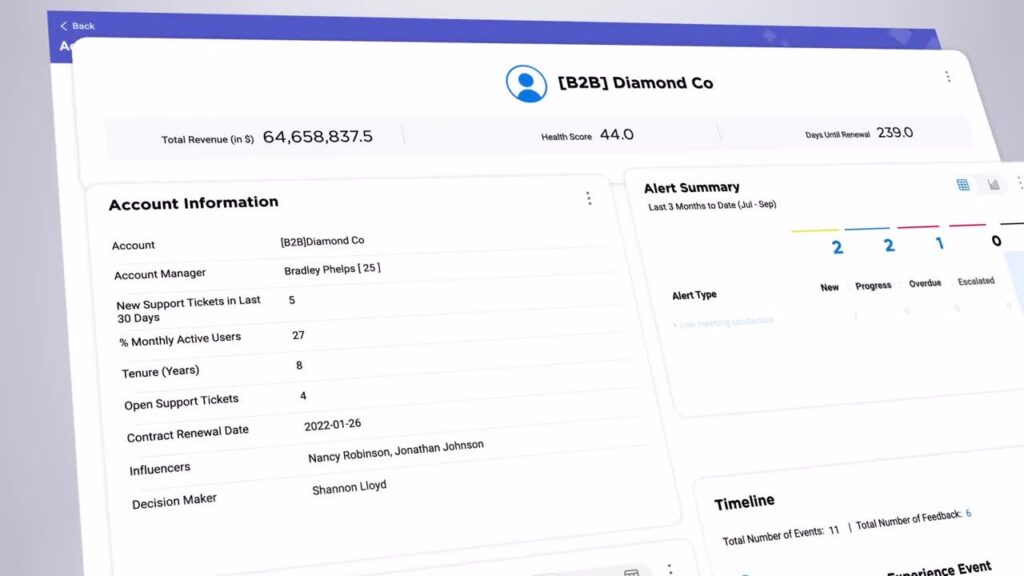
My role has me servicing, upwards of 4 million calls per year from members and providers across 1500 customer service reps. Under my area of responsibility. You can see here on the slide just a little bit about independence. We’re primarily in southeastern Pennsylvania. We call it five County Philadelphia region.
We’re mostly a locally based blue plan, but we have a national footprint. You can see with 8.4 million members, 31 billion in revenue. And [00:02:00] over 14,000 employees. Just real quick about myself I’ve been with Independence Blue Cross for 26 years. I’m an operations lifer. I have been in call center for over 20 years and I’m passionate about the work we do supporting our members and providers.
Chris Brainard: Chris Brainard, I lead the office of patient experience and engagement for UAB Medicine. We are an academic health system. Headquartered in Birmingham, Alabama. We’re associated with the University of Alabama at Birmingham, which is part of the University of Alabama Education system. So many of you may know of our football team, or if you’re a March Madness fan, our basketball team, because we’ve now apparently become a basketball school also, but excited to be here.
UAB is a growing health system. We serve the greater state of Alabama. We’re headquartered in Birmingham with the eighth largest hospital in the country. Over a 1200 bed academic medical center. We’re a level one trauma center. We [00:03:00] have a number of faculty members and physicians, and we’ve recently acquired another local hospital system in the Birmingham Metro area, five hospitals.
And so we’ve grown to be a network of 11 hospitals with over 3000 beds. And so we do a significant amount of care both in the communities and in the rural communities, but also in the greater metro area of Birmingham. Our team in Office of Patient Experience, we really focus on how do we really align the organization around listening to our patients and families, and then turning those insights into actions and strategies through collaboration with our leadership.
Really to drive the health system forward around around the patients.
Elizabeth Cleek: Chris, why don’t you share a little bit about your vision for creating a system that puts people at the center of the healthcare experience?
Chris Brainard: Y’all have been here at the conference this week and we love the Medallia Conference and we’re honored to be working with Medallia and we get to interact with so many different brands here at the conference that I always find very interesting learning [00:04:00] from out of industry, but if you work in the healthcare environment or.
If you yourself have ever been a patient of a healthcare system you realize that the things that happen in a health system might be a little bit different than happen in a retail organization or a hospitality organization. And so the work that we do is high stakes and it makes lasting impacts in the lives of the people that we care for and serve.
And when we think about our vision or what we’re trying to accomplish. Our team always focuses on how do we humanize the healthcare experience and then how do we connect our team, connect their hearts and minds to the work that we’re doing? And so often that starts with this idea of, like Elizabeth said, putting the patient at the center of their healthcare.
And one of the things that’s always a challenge that we think about for our team, when I think about what the ideal patient experience might be like, is that when we serve our patients, you have to really understand those people as individuals. The journey that they’re on [00:05:00] changes. And what I mean by that is, if we have a patient that walks through our doors and they’re seeking primary care, their needs, wants and desires are very different than maybe somebody who’s been in a motor vehicle accident who needs trauma care, or somebody who’s maybe in search of a transplant or neurosurgery and.
The more unique thing I think that’s about healthcare, and I was talking to some of my colleagues who were in other industries the other day about this is you as an individual actually might hold multiple personas if you think about it, right? So you as an individual, if you’re healthy and and you just need a primary care doctor, you’re engaging with our system and you want it to be what I call high speed, low drag.
You want it to be simple and easy and connected, and you want telehealth and it to be digitally enabled and. You want it to be convenient to your house you don’t wanna wait. There’s some things that happen in that primary care space. However, if you receive a cancer diagnosis, I’m guessing if you thought about it, [00:06:00] your needs, wants and desires changed dramatically, don’t they?
You want to make sure you got expertise at your fingertips. You want people who are gonna help navigate what is now gonna be a very complicated journey that’s gonna interact with your whole entire life, right? You’re gonna maybe want counseling services and nutrition services and exercise coaching.
There’s so much more in this broad ecosystem of healthcare that as an organization we have to understand the person that’s in front of us, but we also have to understand the journey that they’re on. And so listening across that journey, they’ll truly understand it makes a big difference. And actually, Michael and I were talking while we were prepping for this, and I was like, I love the fact that we’re both up here, right?
Because. He’s worried about members and I’m worried about patients, but it’s the same person. He’s in Pennsylvania and I’m in Alabama, so it’s not the same person, but you can get what I’m saying, right? The same human is at that intersection of what the insurance company’s doing and what the health system is providing.
And so how do we actually care for that person [00:07:00] based on what they need? And so when we think about delivering that ideal patient experience, it’s really about how do we understand that? But then how do we drive operational change? Improvement team member engagement, like we heard Denise talk about this morning.
And infuse those individuals with the right ideals so that they can actually execute the vision with the patients and families.
Elizabeth Cleek: Thanks, Chris. I think that was a perfect segue into thinking about that patient and member. And so Mike, how do you put the patient or that member at the center?
Of their care.
Michael Lentz: Yeah. Yeah, Chris so great response there. And I would say from the health insurer lens we view ourselves as that like third leg of the stool, if you will. So you have the provider, you have the member, and then you have the insurer, which is the enabler of making sure that access experience and education really is at the forefront of what we do.
And at Independence, it’s really [00:08:00] grounded in our mission which is enhancing the health and wellness of the members and communities we serve. I’m not trying to do a commercial for my company, but we’ve been in business for over 80 years. And we take pride in the bond and the relationship with our community and the members we serve.
And we know a catalyst of that is the relationship we have with our providers. I. We obviously as a Blue Cross Plan have, a national network, but like our homegrown partner providers in the Philadelphia region is what we call second to none. We have great partnerships that we leverage with, children’s Hospital, Philadelphia, university of Pennsylvania Health System. And we really put into practice that partnership and that advocacy for the members we serve, based on our stature in our community and driving forward with our mission. So like Chris focused on provider [00:09:00] patient we’re focused on member.
And of course that provider relationship and making sure we can be that enabler to bring that that partnership in a trusting and lasting way. Removing barriers and obstacles along the way.
Elizabeth Cleek: That’s great. So those are both really big visions, seeing the person in front of you, seeing the patient in front of you.
Having that relationship with the clinicians and with the patients. So how do you realize that, how do you said, Chris, you’re an operations a person. How do you operationalize that vision?
Chris Brainard: I’ll tell you. In a big place like UAB health system it’s complicated, right?
And so we try to simplify it into a few key elements. I always think about things in this mindset of what I call strategy structure, execution, right? What are we trying to accomplish? What is the process by which we’re gonna accomplish it, and then what are the things that we need to execute to, to do that?
And you have to almost reframe that lens every time you’re trying to solve a problem. One of the things that our team has really [00:10:00] focused on over the last five years is we partnered with Medallia really out of a need to for this desire to be nimble and adaptive when it came to listening to people.
Those of you that work in a healthcare environment, we’ve got CMS. We’ve got cap surveys. There’s some things that we’re mandated to do in the government, in the government realm, and just between us. Some of that’s a little clunky. Some of it’s a little cumbersome.
Mailing a scantron to somebody’s home that’s four pages long is not really an ideal way to get data. But now they’ve embraced email and so we’re making small steps forward. But this idea that we could listen in real time with a company like Medallia really helped us, right? So we could embrace text messaging, we could embrace email, we could leverage QR codes, we can get what I call rounding feedback, where we have a live link.
We can go out and talk to people, we can capture data that way. And so the steps to realize that we’re really about how do we get the right information at the right time to inform better decision making. And ultimately better, [00:11:00] better outcomes as an academic health system. We have a research mindset and so we’re always thinking about like, how can we learn from what we’re listening to?
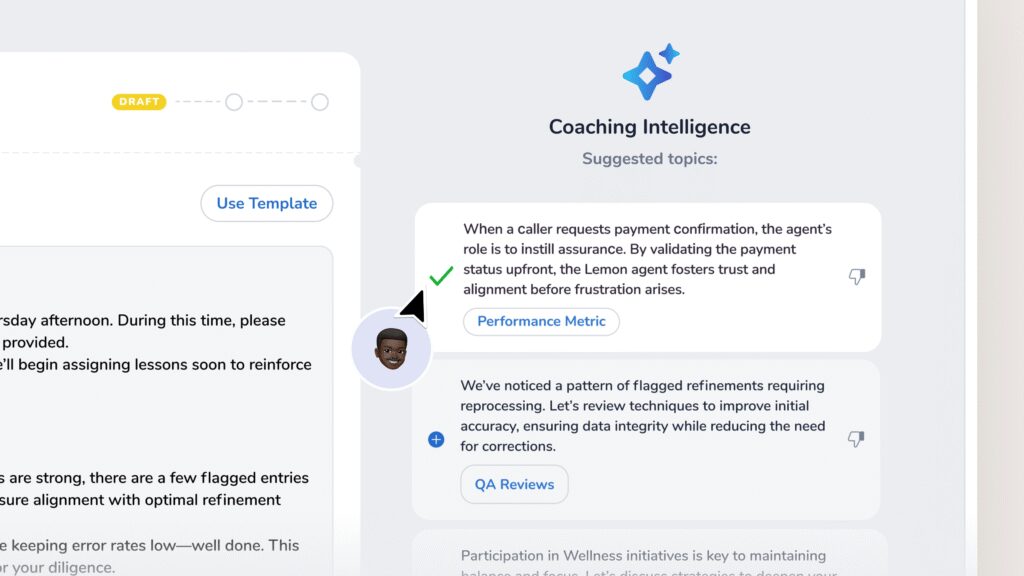
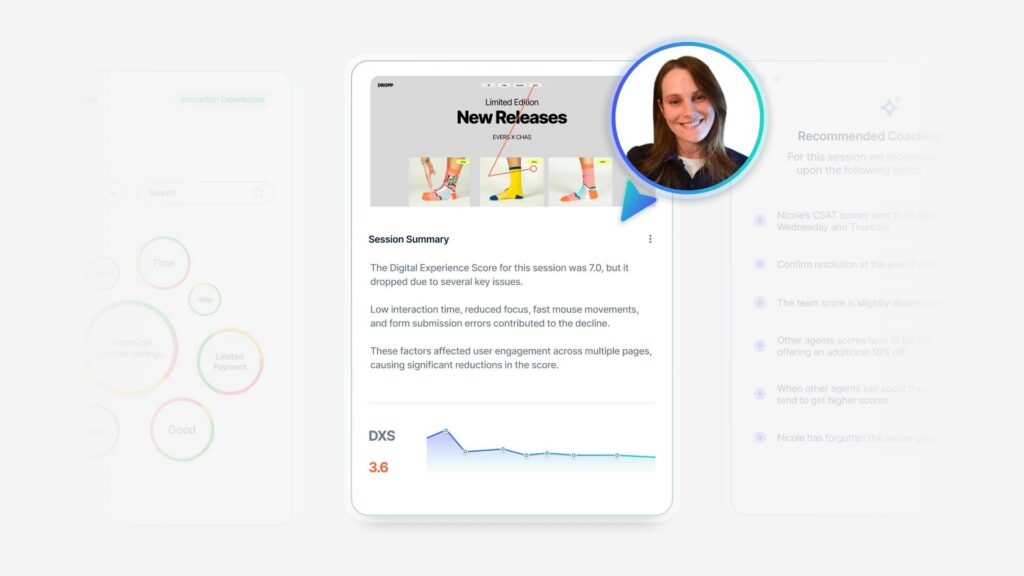
And so I’m really excited personally about some of the advancements that Medallia has started to share around. I. Leveraging AI to read unstructured feedback. And to me that’s really the future, right? Some of these emotions, needs, wants and desires, things that bring us either frustration or joy, those things show up in conversations.
And so I’m really excited about that being something that that we can get into. But taking the listening, so what I’m gonna call quantitative qualitative data from surveys. And turning that back into operations to inform decision making has been one of the things I feel like has helped our organization move ahead with our partnership with Medallia.
And we’ll talk a little bit here about this trust measurement that we’ve embarked on, but, really tuning the organization around this mindset of being the trusted healthcare provider. In my mind, I think about it as how are we the top of mind, [00:12:00] first choice. For a patient when they need healthcare.
And if that starts with delivering on the promises that we make, we really have to make sure that we understand that person in front of us in order to do that. And so leveraging data partnering with operations. And then I think the last thing that, that I’m proud of the work that we’ve done is we take this mindset of really involving the frontline team members in designing improvements and enhancements.
We go out, we’ll talk to the actual frontline team members, the physicians, the nurses and really seek to understand, what it is that they see. And then merge that with what we know the patients are trying to tell us also.
Elizabeth Cleek: Yeah. Thanks Chris. Can you share a little bit more about the Medallia goal team?
Is trust tool, how you’re using? Absolutely.
Chris Brainard: So back to that research mindset. So I was so excited Elizabeth and the team at Gold. And the team at Medallia, we got together and we had this aha moment where we were all of like mind, talking about this concept of [00:13:00] trust. And I don’t know how many of you have ever been a patient, but I’ve been a, I’ve actually been a patient, not at our hospital, but there was a point earlier in my career where I actually was in a hospital bed with a physician standing in front of me saying, you have to go somewhere other than here to save your life.
And you have three choices. Where will, where would you like me to transfer you? And at that point in my career, I had this sort of aha moment where I had to make a decision that was critically high impact. I had no information to make it. And it was all about the reputation of the organization in order to make an informed decision.
And so that’s really shaped the work that, that I’ve done in my career. But this trust tool only came around. And this idea of what are the behaviors, what are the things that providers, if they do them. We’ll actually garner more trust with patients. And we all know if you trust your provider, then you’re gonna most likely do the things that they prescribe you to do, which means you’ll ultimately get better down in the long run.
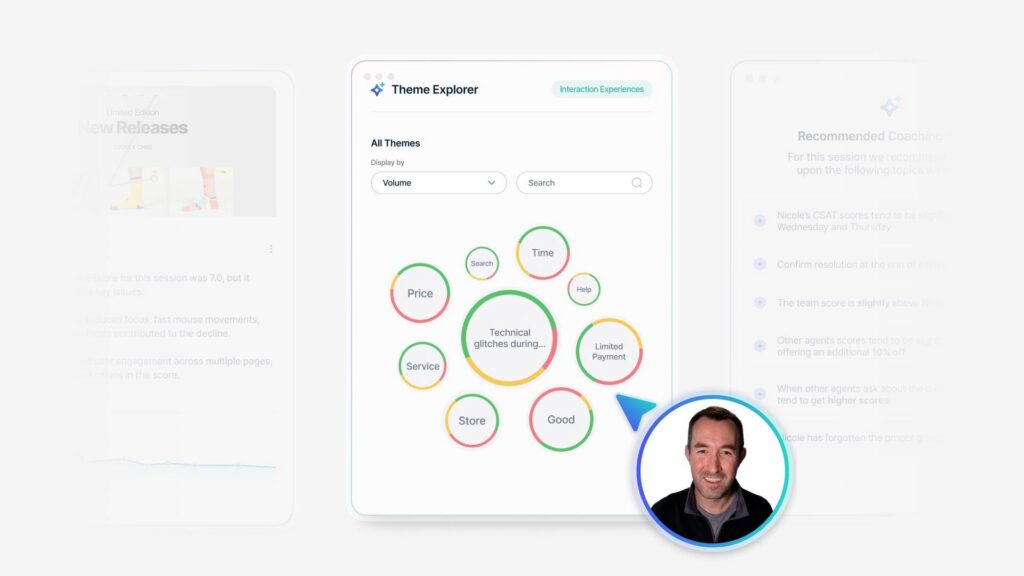
And so we we took the six questions [00:14:00] set. We infused it into what our regular cadence listening strategy was in our primary care practices. And we started to capture that data. We’ve always asked questions around provider communication and. The likelihood to recommend that promoter score things about access The trust tool really gave us this ability to drill into what I’m gonna call prescriptive behaviors.
What feelings did the patients have based on what the providers actually did when they were interacting with ’em. So we started capturing that data, but I’ll let Michael continue to talk about that, but I’ll come back to some of the results and things that we’ve learned through that process.
Michael Lentz: From my lens being operationally focused, like our vision is around our customer experience, north Star. Like probably most in my position, you have to set a vision. We’re focused on supporting the whole person acting with empathy staying a step ahead and keeping it simple.
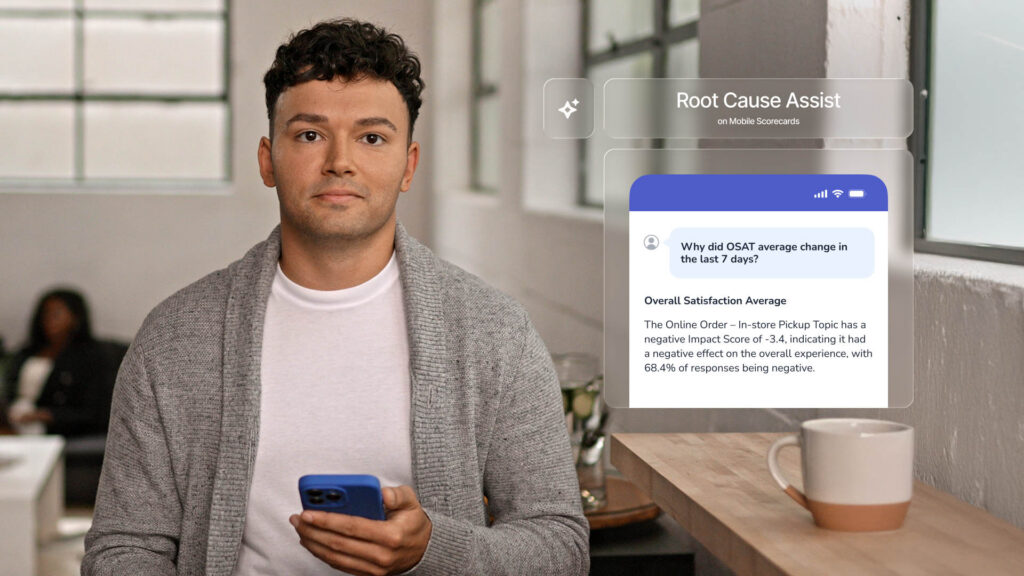
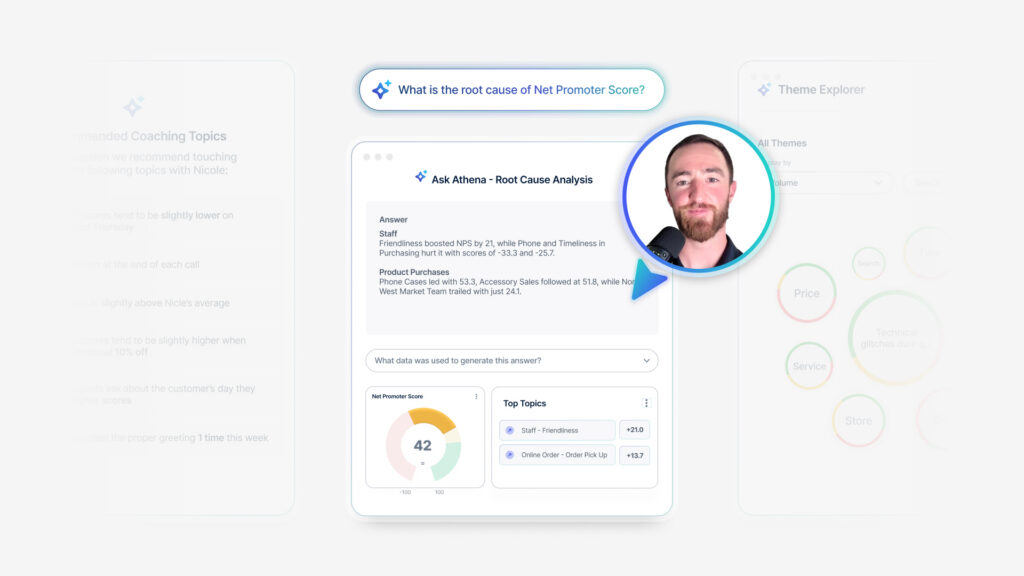
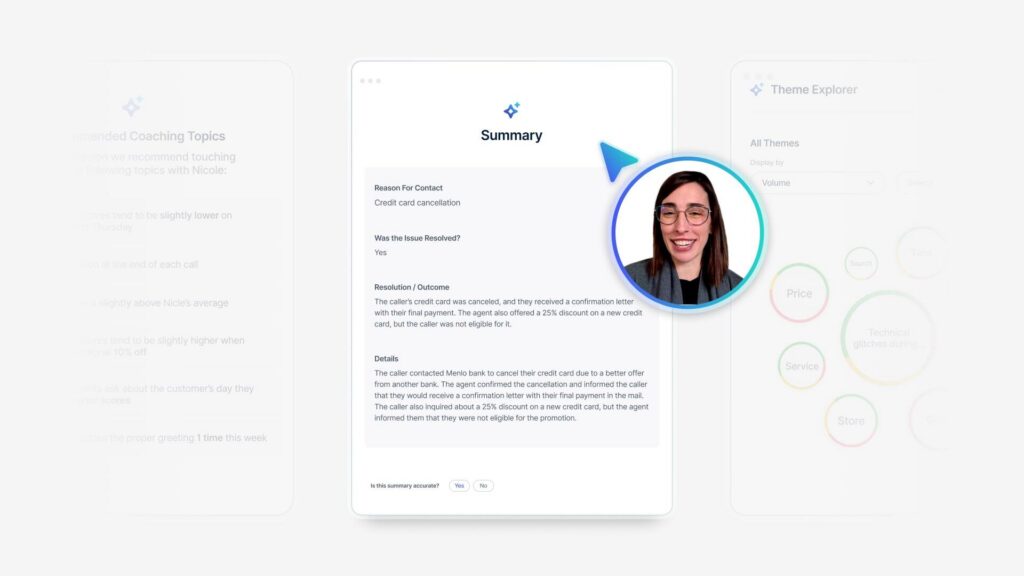
So they’re good aspirations, right? But how do you measure that and how do you use tools [00:15:00] like Medallia? To bring that to reality. So knowing we have those, kind of vision statements and priorities that we’re focused on, we’ve actually been able to use Medallia in different ways to mine the transcriptions of our calls to get an understanding of are there situations where we are ignoring someone providing us with.
Constructive feedback or are there negative sentiments in some of the call transcriptions that we need to raise up maybe to a different point of contact? What we’ve been able to do with the Medallia tool is create those queries that have enabled us to bring those types of things to the forefront.
I guess really for two reasons. We want to, number one, of course. Remove that barrier, resolve the reason for that, negative interaction. But we also wanna make sure we’re using it as a tool for training. We [00:16:00] have a multitude of different business lines. We have Medicare, we have TPA, we have MedSup, we have commercial, we have Medicaid.
We pretty much run the gamut of products and lines of business. And the needs are different obviously across that. We do at the end of the day, feel the vision that we have in terms of customer service delivery and the foundational elements that that a tool like Medallia offers us, gives us that lens that enables us to focus on where we may be doing things incorrectly or, need refinement.
But you know what I also like to tell my team too it’s about. The thousands of things we do well as well. And we should be identifying those and celebrating those things too. And again, like I’m, I have one of my colleagues in the room here, Tyler, and we’re a little bit newer on the Medallia journey.
I’d say within the last two [00:17:00] years we’ve really gotten to a point where we’ve implemented the tool. But for me, it’s it’s being able to have just real time intuitive text analytics on our calls, looking at the transcriptions, focusing on these different layers and visions that we have.
And I’m a big promoter of the Medallia tool in that way. Just how easy it makes it and how we’ve been able to evolve it, really over these last nine months has been pretty incredible.
Elizabeth Cleek: So I’m actually gonna follow up on that and say, so you talked about looking at the whole person, you talked about empathy training.
Can you give some sort of concrete examples how you’ve either used the Medallia tool or how you’ve done that? How, yeah. How do you drill down?
Michael Lentz: Yeah. Yeah. Great question. So I. So when we talk about empathy, we have key words in the queries that we use in Medallia, such as surgery, procedure. We also look for sentiments of frustration, speak to a [00:18:00] supervisor.
We’re able to kinda look at that across different lines of business, but also at a very granular level if we have. Like our Medicare population, they obviously have different needs. If we have a new customer that we’ve brought on, we, of course wanna, make that great first impression.
I. Really I hate to oversimplify it, but it’s just made it easy for us to do that. I would say a real life case too recently is we’ve migrated from an old claims processing platform to a new one. So we’ve created a lot of disruption for our members. We have all new member ID numbers.
We had to reissue all new ID cards, and that in and of itself is a barrier to care because. To get an ID card. We’re relying on the US Postal Service. We do offer digital versions of the ID cards, but like we’ve had to really look deeply into [00:19:00] the different disruptors that we’ve caused as a result of that platform migration that we’ve done.
And we have really done a, what I would consider a really good job. Using the Medallia technology integrated with the call transcriptions that we’re receiving to like mine and suss those things out. And I feel like prior to Medallia, like we did something like this about 10 years ago.
And we have really been able to be proactive and we’re like, wait a sec. Joe’s Pizza has called us at a much higher rate about x and those types of insights, got brought right to the surface and enabled us to look into it and do things more proactively in terms of like issue resolution.
Whereas in the past we would handle ’em almost like on a one by one basis. And if something bubbled up from a. From a service perspective we would deal with it at that [00:20:00] point. So I truly feel that putting that into action has really enabled us to be a little more proactive as well.
Elizabeth Cleek: That’s great. And Chris, I saw you nodding along him.
Chris Brainard: Yeah. I’m just like I love learning from what Mike’s doing and on that side of the business in a tactical space, there’s a lot of things that we’re working on. So I think to help boil the ocean on this one when I think about the experiences our patients have in our ambulatory environment, we see well over.
2 million patient encounters a year. And so we listen across all of those channels and platforms with Medallia. And so you, as you can imagine, we have, data by clinic, we have data by service line, we have all the demographics of the data. But how do you actually take that and start driving it down to what actions should you take with the insights from that sort of grand scale?
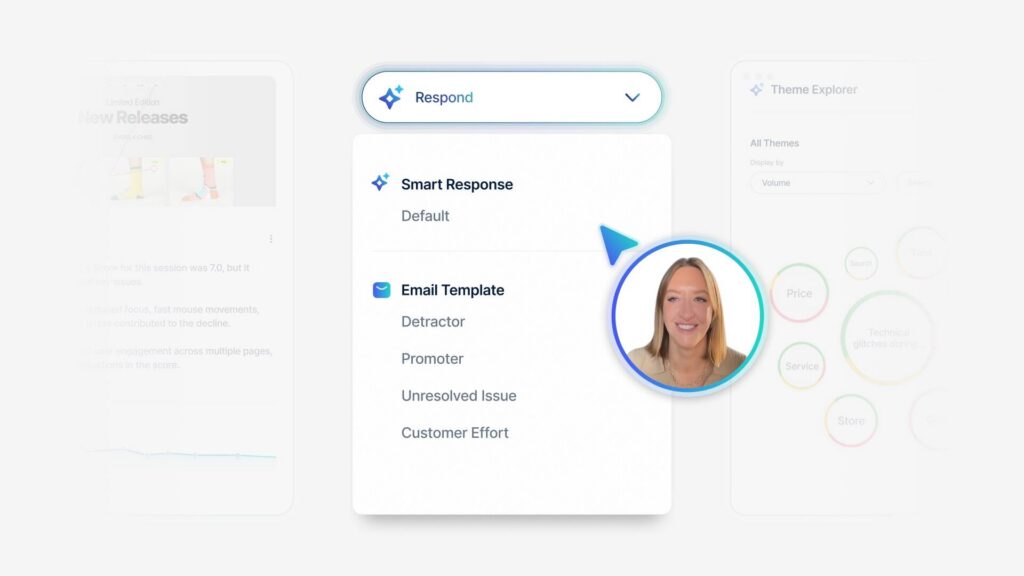
And so what we’ve tried to do is we’ve tried to really distill the information in a way that we can equip the frontline managers. To use it to drive the things that we wanna drive. Simple example, close the loop. A manager’s gonna get [00:21:00] pinged when a patient gives a less than stellar score on the likelihood to recommend they can follow up in real time and solve the problem.
And I could tell you a countless amount of stories of examples like the one where on our old system I would’ve never known that you complained about the cleanliness of a dressing room on the Medallia system. We had one example that always sticks in my mind where. I was drinking a cup of coffee about seven 30 in the morning in my office.
I was reading comments. I found one where somebody complained about a dressing room that needed to be cleaned up from the day before. This is before the practices of open for the day. I sent it to one of our leaders who then had to find this dressing room because it was in an obscure building. As you can imagine, we cover about 14 blocks of downtown Birmingham, so we got lots of places for things to hide.
Found the dressing room. Had it cleaned, replied to the patient and we told that story on a call at nine 30 in front of leadership. And so the speed to action of how you actually fix, find and fix issues with [00:22:00] medallia’s is key. I think that’s an example of taking it to tactical. I. The other piece of taking it to tactical is the Medallia Gold Trust tool.
I think oftentimes when we think about our providers they do amazing things. We have incredible providers. As a matter of fact, in our ambulatory network our average net promoter score for our medical practice is somewhere around 93. So it’s very high. And so we took the Medallia data and we started to identify who are our top doctors when it comes here, and apps from a communication perspective.
So we looked at, hey, anybody who’s got. A 95% or greater on their provider communication domain, and we throw a big party. We invite ’em. We tell ’em to bring their family, their friends, their colleagues, and we just celebrate ’em. We have over 475 providers, give or take every year. They get that recognition.
What’s crazy though is there were 108 providers this year who had a perfect 100% top box score. [00:23:00] Okay, what does that mean? If you’re a provider and you’re seeing patients in your clinic every single day, all day long, and we’re sending out surveys to patients randomly that have interacted with you and they fill them out, that means that not even one time in the course of an entire year off a randomly selected population, does somebody give you less than a nine or 10.
To me, that’s insanely good because that’s like perfection in action, right? So we celebrate those people. And really give ’em a big shout out because that’s the kind of thing that actually drives our brand reputation for excellence, right? That’s the kind of thing that drives trust when it comes to the trust tool.
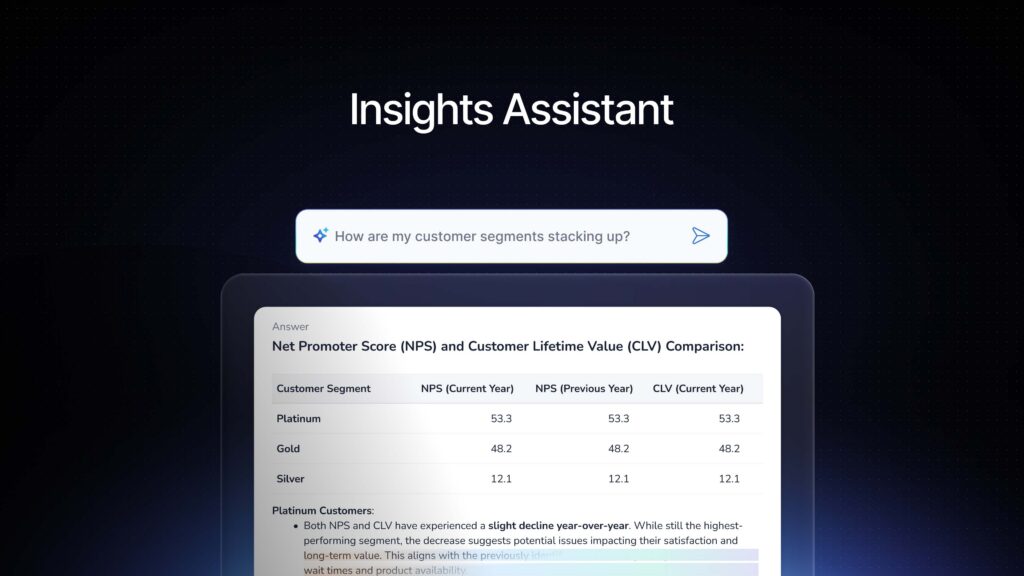
We, when we infuse that into primary care, what we’re trying to do with all of this data is what are the prescriptive actions that we could then take to people and say, Hey, if we do more of this, it makes things better, right? So if you’re a good communicator, do more of that because patients like it. When we did the Medallia Gold Trust tool, what I thought was really interesting, I’m sorry, I don’t like to use notes when I [00:24:00] talk, but I cannot remember this many numbers, so I’m gonna just re But we put that six question set on there and then we did a statistical analysis of, what was the impact of those things, right?
Hey, if as an example, if you show care and concern, what’s the impact of that? If you. Patiently listen and address questions and concern. What’s the impact of that? And what we actually found was on patiently address questions and concerns in a primary care environment if a provider does that well.
So at the top box, the odds are that your patient satisfaction’s gonna improve by 34 34 times. Okay? So super high impact. One action. Super high impact again, if provider patiently addresses questions and concerns with their patients. Likelihood to recommend goes up 13 times. Okay. The perception that our providers actually care about the patients goes up 33 times just by listening and patiently addressing questions and concerns.
If they do that behavior, our [00:25:00] patients felt included in their care, it was likely 23 times more that they felt included in their care. And then last but not least. If a provider patiently addresses questions and concerns in the room of the patient felt heard 15 times more. One behavior drove every single other measure that you might want to drive.
And so I think when we think about how complicated healthcare is and how do we actually put tactical behaviors in place that make an impact, you gotta simplify things, right? It’s like I can’t walk into a provider’s offices and start you need to change all this stuff. It’s Hey, there. Busy.
They’re experts. But if we can take the behaviors, what does patiently addressing questions and concerns in a busy practice really look like? What does it sound like? I. What are the nonverbals, what’s the icon? What’s the words that I say? Where do I position my body? Where’s the computer screen in the room?
Unpacking that one simple question to find those best practices and the things that [00:26:00] those individuals who perform the best that really do. So I see that as the future. Right now we’re making it tactical and practical, and you can go to a provider and instead of just saying Hey, we need our satisfaction to be better, and they’re like, Hey, I’m saving lives over here.
That’s not maybe the key thing I’m worried about. We can say, Hey, if you can slow down just a minute, if you can patiently address your patient’s questions and concerns so they feel heard and understood, actually you’re providing better medicine, right? You’re actually building a better relationship.
You’re actually creating and generating trust with that person. And so that’s the kind of process that we try to undertake with the work that we do.
Elizabeth Cleek: Thank you. I know we’re, the time is moving very quickly. And you’ve both shared I. A lot about the work that you’re doing that requires a huge level of commitment.
You talked about listening to the employee. You talked about getting clinician input and staff input into ways that, that your organizations can improve. Focusing on the patient, the member, [00:27:00] that is a culture change or it’s a whole culture that you’ve both put in place or that your organizations have put in place.
Requires financial commitment, requires buy-in at every level. So in, five seconds or less, tell us how you did that.
Chris Brainard: Mike, you Yeah. Yeah. Mike.
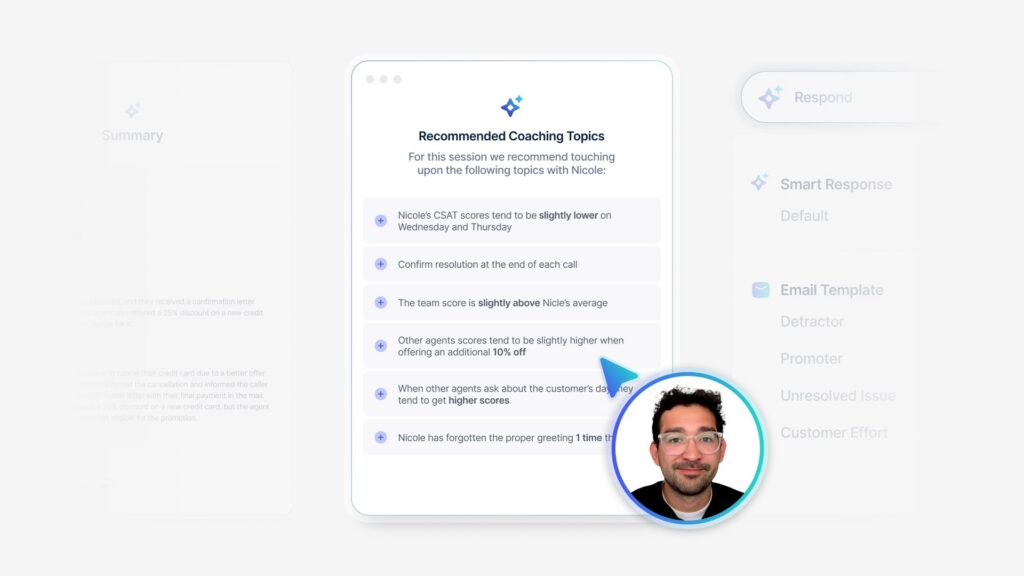
Michael Lentz: Yeah. Yeah. So I feel like one of the biggest things we did that was successful is rallying the organization. So like we call ’em champions. I’ll take the Medallia implementation as an example.
I mentioned that we’ve been on the journey for about two years now, and. It came to us as like we are moving forward with this. We needed to identify key stakeholders in our organization who are gonna be champions to promote the tool. And it really needs to happen from top down. People like myself, counterparts I have in the organization and our member experience in marketing areas need to be promoting the use of the tool and.[00:28:00]
In what we do, what I present, what, people on my team present, all needs to be done cohesively as well, using the Medallia tool and queries that we have. I feel like that’s been a game changer for us is that kind of notion of champions. And it’s not just that. Our analysts use it, or there’s, these canned reports that get generated that nobody really pays attention to.
Like I’m actively talking about it on a daily basis. I’m sending people different queries or insights that we’ve gleaned from calls we took yesterday, calls that we took today, calls that we took last month. Those types of things I think are super powerful. And get others on board now. The tool needs to cooperate, right?
So it needs to be intuitive enough for people like I’m not a very smart person, right? I need to be able to use it, but people who are [00:29:00] maybe a little bit smarter and good with data also need to see the value in it as well. And I feel like it just checks all the boxes for us. One thing that’s been huge for us and I attribute it to the work we’re doing in NA is Chris talked about, CAP scores with Medicare.
We’re focused on member experience for our Medicare population. We’ve been a five star Medicare plan two years in a row for our HMO contract in 2022 and 2023. We’re four and a half star. I’m focused on our CAP scores. So last year we were a five star customer service organization on the star ratings for that specific measure.
For our HMO and PPO contracts, we went up by a point and a half percentage wise on our FCR scores based on our post-call surveys. I attribute that to the work we’re doing with Medallia [00:30:00] to, as I said, suss out these dissatisfiers aligning to the visions that I had set forth with.
Focusing on the whole person acting with empathy, EE, et cetera. It’s been a game changer for us and I really feel like it’s I was gonna talk a little bit about the future as well. So I’m excited to be here because one of the things I’ve been, I don’t wanna say complaining about, but like in today’s world, you can go on Amazon and you can see the reviews, but it summarizes the reviews for you right there.
I. I’m so excited to see that there is a capability. And I, it was covered in the keynote yesterday where Call Summarization is now a reality. I get asked, I can’t tell you how many times a day, what are members calling us about? What issues are we seeing here? The way we do it today, outside of the queries we developed is we’re mining call transcripts and we’re listening to a bunch of calls.
My area handles about 30,000 calls a [00:31:00] day, so imagine. How many calls you could possibly listen to or how many transcriptions you can read. So that’s where our future is to really use some of those tools as well with call summarization specifically to help us get to the crux of, where our opportunities are or also what we’re doing well too.
Elizabeth Cleek: Thank you. I know we’re close. I wanna get to some questions, but I really want to hear what you have to say on that first Chris, in terms of
Chris Brainard: on, on the future.
Elizabeth Cleek: On in terms of how do you creating culture is huge. Wow. And you’ve clearly done that. So how
Chris Brainard: I’ll tell you, we, we’ve been on this journey for for a long time.
I’ve been at UAB, it’ll be 14 years. Next week, and we’ve been on the journey the whole time, and I think that’s sometimes part of what you have to keep in the back of your mind is it’s this kind of continual disciplined, forward momentum time and time again. Sometimes you have to back up and reeducate.
[00:32:00] Sometimes you have to back up and redesign. But you have to continue keeping the main thing, and keep it moving forward. And I feel as an organization, it’s been great over the last 14 years. We’ve navigated, different executive leaders. We navigated covid, we navigated mergers and acquisitions.
Every time I, think through what’s gone on over the history of the organization, but during that entire time. It’s like painting the Golden Gate Bridge. We have focused on how do we become a better place for our patients and our families. And my mantra has always been experience management early in my career was really about that outcome measure.
How are those HCAP scores? What’s the top box number? And all that mattered was, is the number, right? So that, we get the, hit the goal and get the incentive paid to the executive. Versus what my belief system has always been is how do we put the voice of the people on our team and the patients we care for at the table so that we actually design better [00:33:00] healthcare for the future off of what they really need and want.
And so Medallia, I feel like has really helped us do that exponentially. I tell people all the time, I feel like we moved 10 years and two years when we implemented Medallia. Because it actually gave us the ability to be nimble, adaptive, and actually put the voice of the people and the patients in the room we’re not perfect, first of all.
There’s still stuff we’ve gotta fix and there’s still things that we have to influence differently, but I’m thankful that the organization has believed what we believe as far as what as far as that goes.
Elizabeth Cleek: Thank you. That’s great. 10 years and two years. That’s a stat. So I do wanna open it up to folks.
Does anybody have a question? And if, oh, okay.
Q+A: You had just mentioned being, going from this, people being very focused on that top two box and what is an NPS number, et cetera. I just started at a company and we’re there. Everyone is so focused on. Like NPS. [00:34:00] N-P-S-N-P-S. And so I’m wondering what advice you might give for someone who’s trying to go in and maybe add extra information, like trust and what’s important from the clinician kind of perspective when you have an organization that’s so focused on that one number.
Sure. That’s a great question.
Chris Brainard: Yeah, so my advice on that one, I mean I think goals are important, so let’s not discount, we say goals in our organization and I think it helps to keep people focused on things. The qualitative feedback though, in my opinion, is where the real goal comes in. And so while the numbers are good to monitor and you can drill those things down, to a clinic or a work group or a journey, what are the patients really saying in those surveys? And how does the team. Hear the voice of the patient. So a couple opportunities that you could leverage if you’re a Medallia client.
I think one thing that’s been big for us is we use Medallia video. So I start meetings with a video of our patients. Not all of them are [00:35:00] positive, so we share some of the negative ones, right? But we also share the positive ones and I’ll send those. And I actually, I can tell you a tactical story. What I mean by that is I was, Monday morning, I was looking at some living lens videos and I saw one on a provider that I knew.
So I sent it to him in an email, and this is like at eight o’clock in the morning and he sends me an email back, like immediately. I was on call this weekend and it was rough. This made a huge difference. More than you’ll know, right? And I think that’s the kind of stuff you have to think about. It’s take, stop the number.
You gotta track the numbers, but you gotta turn it back into like, why are we here and what do we do? And I think sometimes in healthcare, it’s like we get so busy in a boardroom talking about stuff. It’s like, why does our business actually exist? And what are the people who wake up every day showing up to actually do here?
And then how do we connect their purpose and passion with our work? And I think that listening to the customer is actually what they want to be doing. And so how do you make that easier for them to really [00:36:00] hear from the, in our case, the patients.
Michael Lentz: Yeah. Yeah. And if I could add to it as well from what we do on the.
Inbound call side. Like NPS of course is all the rage for us as well. And we focus on it every day. That’s the key. We can’t look at it a month ago. It’s gotta be a daily focus. And the way we do it is whoever the detractors are, what comments have they left? Can we validate or substantiate those comments by listening to those calls?
And then we decide is it a, is it a skill issue, maybe at a rep level that we might need additional training or reinforcement, or do we have something a little bit more globally with a broken process somewhere? So I feel like those small components have made a huge difference for us in focusing on NPS.
Of course, we want to continue to improve. We’re not where we want to be, but our daily focus on that and focused on the detractors. We are also focused on the [00:37:00] promoters, but. Has really helped us tremendously.
Room Host: Thank you. I think we probably have time for, okay. I see. One more question. Oh, two. Okay.
We’ll try.
Q+A (2): I’m Raymond Dramas from Williams Sonoma, a retail company. And since you mentioned about being nimble and adaptive, we’ve all, we’ve just started to use this alert functionality of Medallia, so we’re very new to it. I would like to ask, how have you used this functionality and how do you prioritize which alerts to work on?
Is it based on NPS impact or negative sentiment? Just wanna know your thoughts on that. ’cause there could be so many things that you know could go wrong. How do you fo which one do you focus on?
Michael Lentz: I’ll take it real quick just from my lens. So to me it goes back to our priorities. I talked about our kind of vision, empathy whole person [00:38:00] health, tho those are the flags we focus on as it relates to what pops up in the data.
And I would say the second thing is around just the focus that we’re trying to have on NPS. That, that is a measure that we focus on a daily basis, primarily on detractors, because of course we want to resolve those issues, but we want to eventually turn them into promoters.
Chris Brainard: Yeah. My advice would be, what problem are you trying to solve, right?
So we do in our ambulatory clinics where if a patient gives us a zero to three, like it’ll ping somebody and they can call ’em, but that patient’s already left the building at this point, so that’s where we’re at. But where I would love to be would be like, how do we know that something has gone wrong before they leave the building so we can fix it then?
And I think that’s back to the sort of what problem are you trying to solve, and then do you have the integration with operations to put those processes in [00:39:00] place? And so we’re we’re a little bit more reactive where I still think our patients value the fact that they’ve been heard and that somebody took action, because hopefully that means we’ve cut off an issue for the next person.
But I think if to win at the game, how do you use the data you’ve got or the processes, you’ve got to find that issue in the moment and solve it then for that actual individual. And I know your business is a lot different than our business, but. But that’s the mindset I think with.
Elizabeth Cleek: Got it. Thank you both. I do see other questions. I apologize. We are actually over time. If you folks are able to stay for a minute or two afterwards and answer any questions. Much thank you
Chris Brainard: all for your time and attention. Thank you very much. We
Elizabeth Cleek: appreciate it.